Shave Biopsy
Snip Excision
This is a simple and effective treatment for skin tags and some larger fibroepithelial polyps.
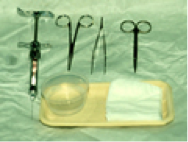
The equipment needed for this technique include forceps, sharp scissors, a haemostatic agent or electrocautery device, and local anaesthetic may be needed for larger lesions.
Histopathological examination is not always necessary but is advisable for the larger polyps as a variety of pathologies can give rise to these.
Technique
- For small skin tags local anaesthetic is not needed as it is more painful than the snip excision. Reserve local anaesthetic for lesions with broader bases when electrocautery is likely to be required.
- Lift the tag from its tip away from the skin to allow identification of the neck of the tag.
- Using sharp scissors, snip the lesion through the neck taking care not to cut the skin itself as this makes the procedure more painful.
- Tiny bleeding points usually stop oozing spontaneously after a few minutes.
- Larger lesions will need chemical haemostasis or electrocautery and should be pre-injected with local anaesthetic anticipating this.
- A simple dressing can be used when larger polyps have been treated but are unnecessary for smaller lesions.
 |
 |
 |
 |
 |
NB – Patient aftercare instructions both verbal and written are helpful.
Shave Excision and Shave Biopsy
The horizontal shave technique is used for biopsy of excision of papular or exophytic skin lesions such as benign papular naevi, seborrhoeic keratoses, basal cell carcinomas and other skin appendage tumours situated in the epidermis or upper dermis. The horizontal shave technique can also be used to take samples of epidermal skin diseases, in particular the bullous dermatoses where lesional and peri-lesional skin can be obtained along with superficial dermis. Other examples include collection of superficial skin for fungal hyphae or epidermal pinch grafts for grafting of leg ulcers. The technique itself is simple and quick and cosmetic consequences after healing are usually very acceptable.
The cosmetic outcome is frequently superior to standard excisional techniques in the management of benign papular naevi. In up to 45% of patients there is no evidence of a scar when assessed six months post operatively and in pigmented and hairy naevi there is only a small risk of retained pigment and hair at the site of the original mole (approximately 25% and 20% respectively)(1)
A variety of tools can be used to carry out the shaving process and include No. 15 or 22 blades mounted on a scalpel handle, a razor blade held between the thumb and forefinger or using a device called the US gizmo.

Because of the vascular nature of most naevi and tumours, it is advisable to use Lignocaine with Adrenaline (or similar local anaesthetic) as the preferred anaesthetic. The methods used for haemostasis include hot beaded tip cautery, hyfrecation and aluminium chloride. The former technique is preferred in benign papular naevi because of the lower incidence of retained pigment at the naevus site, whereas chemical haemostasis may be preferable in tumours, particularly more friable ones, when with cautery one can see tumour burning without necessarily gaining the desired haemostatic effect.
Always use aqueous antiseptic solutions when electrocautery is to be used.
Reference: Hudson-Peacock M, Bishop J and Lawrence C M. Shave excision of benign papular naevocytic naevi. Br. J of Pl Surg 1995; 48: 318-322.
Technique for benign papular lesions such as naevi
- Infiltrate local anaesthetic directly into the lesion to raise it up slightly. Infiltrating the lesion this way makes it stiffer and easier to slice off.
- Using a No. 15 blade mounted on a scalpel handle, or other chosen surgical tool, it is held horizontally and the lesion shaved off flush with the skin using a gentle advancing sawing motion.
- This process is made easier by stretching the skin either side of the lesion to prevent excessive movement during the sawing process.
- Always send the lesion for histopathological examination.
- Haemostasis can be achieved using hot beaded tip cautery or gentle hyfrecation for the best cosmetic outcome.
Technique for shave biopsy of tumours
- Infiltrate local anaesthetic into the area for sampling.
- Tissue can then be shaved from a representative part of the tumour (usually the thickest or most unusual part) and sent for histopathological examination.
- Haemostasis can be achieved using cautery or aluminium chloride, the latter technique being preferred with particularly friable tumours.
Always give clear verbal (and preferably written) after care instructions to patients after the procedure has been completed. This reinforces what should have been discussed when gaining the preoperative informed consent and gives patients more confidence in taking care of their wounds whilst healing is ongoing.
