Wound Healing and Care
Suture Removal
In thin skin, such as the eyelids, sutures may be removed in 1-2 days. On the back, or if under some tension, up to 14 days may be reasonable, but there is a higher incidence of infection. Suture marks are uncommon if sutures are removed in less than 7 days, but almost universal at 14 days.
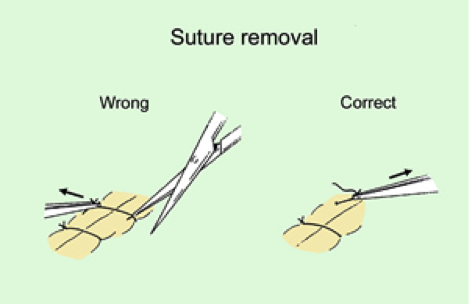
Removal Technique
The surface should be gently cleaned. Cut the stitch with IRIS SCISSORS – NOT with stitch cutting blade, which tends to pull the wound apart. Once cut, pull the suture across the wound.
Suture removal
Dressings for Wounds
Individual preferences for dressings will develop and the following notes are intended for initial guidance. A suitable dressing for a routine elliptical excision might consist of a small strip of dressing gauze placed directly over the wound and then the whole cleaned area covered with a transparent semi permeable membrane such as Bioclusive, Tegaderm or Op-Site. This type of dressing enables observation of the area around the wound without disturbing it. Small wounds may be covered directly with adhesive strips which need to be clean but not necessarily sterile. To obtain this unroll sufficient tape from its roll so that previously covered tape is exposed; cut this off and discard. Use the next portion of tape to cover the wound. Flesh coloured tape gives an almost invisible cover to a small wound.
Antiseptics
- designed for application to intact skin to reduce bacteria
- inactivated by organic matter
- effects on wounds: leucocytotoxic, cytotoxic to fibroblasts and keratinocytes, tissue necrosis, retard epithelialisation
Topical antibiotics
- little benefit in sutured wounds as most contamination ceases with wound closure
- no significant difference in infection rate when comparing white petrolatum and Bacitracin
- regular application may suppress cutaneous flora and select pathogens
- Occlusive wound dressings
- Back as 1960 it was realised that blisters heal faster if left unbroken and wound occlusion with polythene more than doubled epithelialisation
- moist wound healing 40% faster than air-exposed
- epidermal migration facilitated by moist conditions and absence of crust
- increased bacterial colonisation but no higher rate of infection
A good surgical wound dressing should:
- provide a moist environment
- wick exudate away from the wound
- protected against infection, foreign material and mechanical trauma
- aid in haemostasis
- limit motion in surrounding tissues
Dressing design
- ointments – antibiotic, petrolatum
- contact layer – non-adherent
- absorbent layer – gauze pads
- contouring layer – gauze pads, dental rolls
- securing layer – tape, tubular bandage, elesticated bandages
Dressing complications
- excessive pressure – bulla, ulcer, flap/graft failure
- insufficient pressure – risk of bleeding, haematoma
- excessive occlusion – bacterial overgrowth
- inappropriate contact layer – pain and bleeding with dressing changes
Wound dressings
- dressing pads – Melolin, Release, Mepore, Primapore
- alginate – Kaltostat, Sorbsan
- foam – Lyofoam, Allevyn
- hydrogel – Debrisan, Intrasite Gel
- hydrocolloid – Granuflex, Comfeel
- vapour-permeable – Opsite, Tegaderm
Changing dressings
Daily dressing is not necessary for clean wounds. It is needed for excessive exudates but take care not to disrupt re-epithelialisation.
Port Operative Care
Even after a local anaesthetic, some patients will feel faint and need to lie down. At least one couch will be required for recovery. Most patients can remain seated in a chair until they feel fit enough to return home. Ideally patients who are having minor procedures should be brought to hospital and taken home afterwards by a friend or relative. Procedures on the upper face e.g. around the eyes may need dressings which restrict or impair vision.
Many patients feel slightly ‘odd’ post-operatively, and therefore may not really be fit to drive. It is helpful for patients who have had bigger procedures to have some instructions for home dressings. The following information can be used as a patient handout.
