Basic Instruments, Facilities, Sterilization
Instruments
As a general rule instruments for skin surgery are ‘fine’, being smaller and more delicate than general surgical equipment. Always try out the instruments, to make certain they fit your hand well, and clamp and unclamp easily. Avoid cheap instruments as these rust and disintegrate quickly. Tungsten jaws for needle-holders are desirable, but not essential, as they are so hard that they may chip and may cut sutures inadvertently. Plain jaws will hold small needles better than grooved ones.
Ideally left handed surgeons should use left handed needle holders (with reversed ratchet) or use the Matthieu type which will suit either hand. Scissors are also handed, and if right handed scissors are used left handed there is a marked loss of shear and torque forces. The following are recommended.
Essential
Bard-Parker Scalpel handle No.3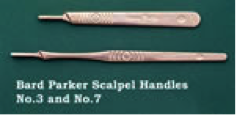
Blade No.15
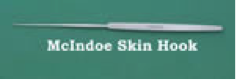
Skin hooks 2 – Kilner, Gillies or McKindoe
Forceps – Fine Toothed and Non-Toothed e.g. Adsons
 |
 |
 |
 |
 |
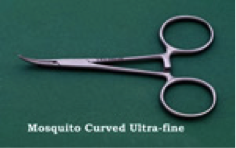
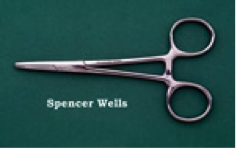
Mosquito Forceps Curved e.g. Halstead (2 minimum)
 |
 |
 |
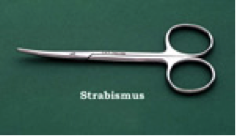
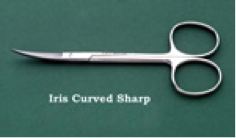
Scissors – Curved, blunt, fine, e.g. Metzenbaum/Lahey serrated Approx. 125-150mm
 |
 |
 |
 |
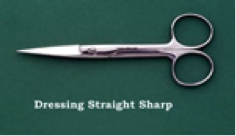 |
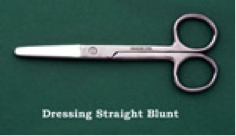
Strong scissors for cutting sutures and dressings
Iris Scissors 75-100mm
Needle Holder – Fine Jaws e.g. Halsey, Crilewood, 125-150mm.
 |
 |
 |
 |
 |
 |
Skin Marker, e.g. Summerlad or disposable sterile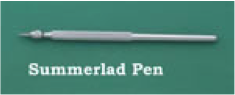
Sponge Forceps
In Separate Sterile pack:
Curettes, e.g. Stiefel Ring curettes 4 and 7 mm
Punch Biopsies 3 – 6mm (usually 4mm) (Stiefel)
Towel clips

Desirable
Cats paw retractor
 |
 |
 |
Chalazion (Eyelid) Clamp e.g. Desmarres (medium)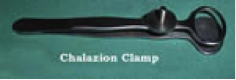
Beaver Handle for very small scalpel blade.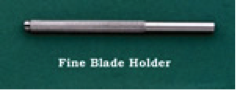
Mono – polar + bi-polar electrocautery
Dental Syringe.
Ophthalmic forceps – small toothed e.g. St Martins

Using Needle Holders
Thumb – Ring Finger Grip
Accurate needle release without pulling on tissues. Precise, rapid, re-gripping of needle for next stitch. Easy regripping of needle. Control not so good as palm grip.

Palm Grip
This gives accurate control. The ball of the thumb releases the ratchet. The disadvantage is that the grip must be adjusted before placing another stitch.
 |
 |
 |
 |
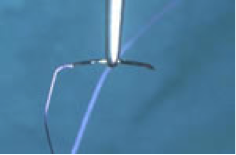
Holding the Needle
This should normally be mid curve. The needle is designed to be held here. Nearer the swage allows greater needle length to be inserted but there is a risk of bending. Nearer the point for tough tissue.
Hold the needle with the points of the needle holder as shown in the diagram.
 |
 |
Facilities, Equipment and Instruments
- To perform minor surgery safely and to a satisfactory standard, the operating room and equipment must meet



basic criteria.
- The room must be of adequate size and used solely for clean purposes. It should have washable walls, floor and ceiling, and be large enough to house all equipment needed. There should be sufficient space for movement around the patient and equipment without the risk of de-sterilisation during the procedure.
- Within the room should be an area for scrubbing up pre-operatively. This must have taps which are operated without the use of hands.
- Adequate lighting must be provided, particularly background general illumination and some form of higher focal illumination on the area you are working on. The Angle-poise type of illumination is not satisfactory.
- An operating table or adjustable couch in which the height can be adjusted, sufficiently narrow for the patient to be accessible FROM both sides. There should be a head end which is adjustable for height and either the foot should be able to be raised or the table tilted to place the patient in a head down position.
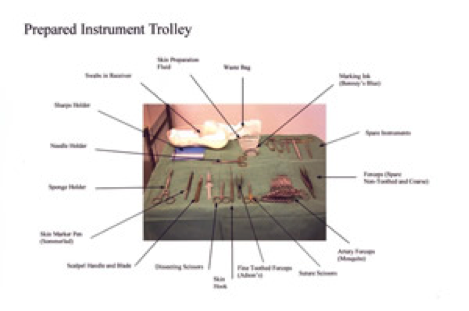
- A mobile trolley with a sterilisable top surface should be available on which instruments will be placed.

- Suction apparatus is useful for some areas, e.g. around the eye.
 |
 |
- Haemostatic equipment, e.g. mono or bipolar diathermy or hot wire cautery, should be available.

- Resuscitation equipment. This should include adequate anaesthetic suction apparatus, which should be tested before each session.
- Intubation equipment. Apparatus for providing intravenous fluids and suitable drugs for resuscitation.
Sterilization of Instruments
All instruments and materials for surgical purposes must be adequately sterilized before use. Pathological organisms including viruses and the spore forms of bacteria must be inactivated. Before a suitable sterilizing process can be used the instruments must be cleaned to remove all organic debris. Usually washing in a detergent and water mixture and scrubbing with a small brush e.g. a nailbrush is adequate. The following methods of sterilization are available, however it is recommended that all surgical instruments are sterilized in a central sterilizing department to ensure consistent quality controls are used, as organisms such as prion proteins require special treatment.
Steam Autoclave is the method of choice. It is reliable and effective, killing bacteria, spores and viruses, including Hepatitis B and HIV. Larger machines (e.g. Little sister) cycle at 115, 121 and 134°C taking around 15 minutes for the highest temperature. Smaller machines often have only one cycle and frequently take 30 to 40 minutes per cycle. The only disadvantage is the tendency to dull the cutting edges of sharp instruments.
Boiling water is not recommended, as it does not kill spores or Hepatitis B.
Chemical Methods. Usually based on glutaraldehyde, which is toxic and may sensitise (see COSSH regulations). These are unreliable for initial sterilization but may be used after Autoclaving instruments to maintain sterility if the instruments are not to be used immediately.
Dry Heat. More effective than chemicals or boiling water but a relatively slow method. The sterilizer maintains a temperature of 160°C for one hour, which may char, burn or melt paper, cloth or plastic. The method is really only suitable for metallic instruments.
Gas Sterilization and Gamma Radiation. These methods are highly effective but only applicable to a very large unit or industry.
A report by the Department of Health (Ref. HEI No. 196: A further evaluation of transportable steam sterilizers for unwrapped instruments and utensils. March 1990) tests small sterilizers, assessing them against British Standard 3970. Available from:- DHSS, NHS Procurement Directorate, Room 423, 14 Russell Square, London, WC1B 5EP. Tel: 071 636 6811 ext 3179.
No single model tested met all the requirements. However, the following have an acceptable performance :- Instaclave, Little Sister 2,Stericube, Sterimate 2000
