Nail Surgery
Few doctors are proficient in surgery of the nail unit. Dermatologists should be familiar with the techniques of diagnostic and therapeutic biopsies of the nail plate, bed and matrix. The important anatomical considerations are shown.
Instruments
Nail clippers, nail splitter, double skin hook and septum elevator (artery forceps will do), in addition to a skin surgery pack.
Anaesthetic
1% Lignocaine ring block and/or wing block (inject at points 3mm proximal to the proximal nail fold in the line of the lateral fold).
Preparation
The digit can be soaked in warm water with added Hibiscrub preoperatively. This enables you to clean away subungual debris, reduce bacterial load and soften the nail. Apply a surgical glove to patient’s hand, snip a minute hole in end of finger and roll back the rubber toward the MCP joint
Nail plate biopsy
This is used to get tissue where there is a thick dystrophic distal nail with or without underlying hyperkeratosis and when a histological specimen might help to identify fungus. Also used when distal pigment could be melanin or blood. Soak nail in water for 20 minutes. Anaesthetic often not required. With clippers or a blade remove chunk of nail. Another method is to do a punch biopsy through the nail.
Avulsion and Nail bed biopsy
Indications for this are tumours, severe dystrophy and unknown lesions. Dissect the attachment of the cuticle from the nail plate using fine scissors. Avulse the plate with the septum elevator or artery forceps (serrated side against the nail), by sliding it from the free edge under the nail. There is a “give” when it reaches the matrix. Grasp the nail with artery forceps and rotate it sideways to free the rest.
To visualise only the lateral half of the nail bed or matrix a partial nail avulsion can be used. Split the nail longitudinally with the nail splitters up to the proximal nail fold. Complete the split with pointed scissors. Half the nail can then be avulsed as before. It is less painful post operatively than complete avulsion. Equally a lesion of this distal bed may be visualised by removing the distal half of the nail only.
The biopsy should be longitudinal and down to bone. The specimen can be spiked with a green needle and should be treated carefully. Suture the wound if possible.
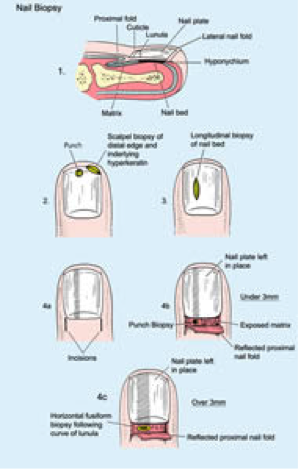
Nail matrix biopsy
Useful for longitudinal pigmented streaks. Remember that in a caucasian a solitary acquired streak may well be malignant. If the streak is near the lateral nail fold complete excision with a broad lateral longitudinal biopsy may be the best choice. Often the plate can be left in place but if you remove it be sure to mark the proximal fold at the appropriate point beforehand. Make bilateral incisions, which extend the lateral folds proximally (by about 5mm). The proximal fold can now be reflected to expose matrix. Biopsy the matrix at the origin of the streak. Up to a diameter of 3mm, a punch is suitable. Beyond that it is best to make a fusiform incision horizontally following the curve of the lunula. Try to suture the defect with vicryl or catgut. Tumours arising in the matrix may require wider excision, but if the diameter exceeds 3mm there is a danger of a permanent nail defect.
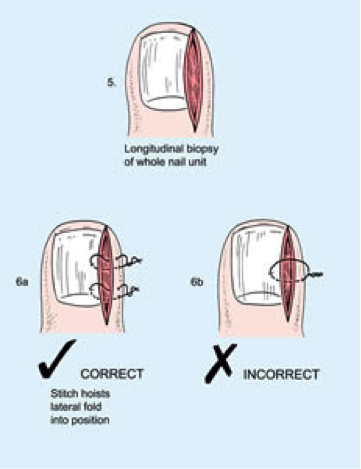
Longitudinal biopsy
It may not be clear whether a dystrophy arises in bed or matrix. A tumour may extend across both. Here the technique is to excise, down to bone, a piece of tissue starting 5mm proximal to the proximal fold and extending all the way to the hyponychium. If the width exceeds 3mm there is likely to be a permanent defect. Suture the wound with prolene. The lateral margin of the biopsy ideally utilises the sulcus between the nail fold and nail. The repair should then hoist the lateral fold up using the backstitch for the best cosmetic result.
Post-operative care. Biopsied nails are very sore and throb. The limb should be elevated for 1 – 2 days. Antibiotic ointment is useful and can be covered with a non-stick dressing, and lightly bound with micropore paper tape. Systemic antibiotic prophylaxis is appropriate in children or when the nail was broken or crusted before surgery. The dressing is changed daily until blood staining ceases.